Understanding the Mind–Body Connection in Healing Pain Introduction: Pain Is a Message, Not Just a Symptom Pain is more than a fleeting discomfort—it’s a signal. Our body’s internal alarm system alerts us to injury, but also to hidden emotional wounds we may not consciously recognize. When the stress, trauma, or anxiety we’re holding in can’t …
Understanding the Mind–Body Connection in Healing Pain
Introduction: Pain Is a Message, Not Just a Symptom
Pain is more than a fleeting discomfort—it’s a signal. Our body’s internal alarm system alerts us to injury, but also to hidden emotional wounds we may not consciously recognize. When the stress, trauma, or anxiety we’re holding in can’t find another outlet, pain often becomes its voice.
Understanding this interplay between emotional and physical experiences is key for healthcare professionals and individuals alike. It allows for more empathetic treatment, holistic outcomes, and timely referrals to psychological support.
1. Pain as Protection
Pain is the body’s natural way of protecting us. A sore muscle or sprained joint tells us to stop and heal. But pain can also act as a protector of emotional wounds—showing up in our physical body when emotional processing is stalled.
In these cases, the pain isn’t “all in your head.” It’s real—but it’s trying to speak a different kind of truth.
2. What your body pain is REALLY saying about your emotions
When our ability to process feelings is compromised—maybe we were taught not to express emotion, or a past trauma left us disconnected—pain becomes a substitute sense.
Instead of saying “I feel anxious,” the body says “I feel tightness in my chest.”
Instead of “I’m heartbroken,” it says “My stomach hurts all the time.”
This shift in perception is not just metaphorical. It’s neurological. And it can deeply impact recovery.
3. Somatic Stress Responses

Stress often doesn’t stay silent. It shapes itself into physical sensations, especially when we’ve been taught to push through or dismiss emotional discomfort. This is what we call SOMATIC symptoms. It’s when the Doctor says the tests look fine, but you can still feel the pain – that’s when you know it’s emotional and not just physical!
Common somatic symptoms include:
- Headaches
- Neck and back tension
- Stomach or digestion issues
- Fatigue and sleep disturbances
- Chest tightness or shortness of breath
Many of these symptoms are invisible in lab results, which can lead to further frustration and emotional suppression—until they’re finally recognized as stress responses.
4. Emotional Triggers Behind Chronic Pain
Our bodies are like sponges—they absorb what we can’t process.
Over time, unresolved emotions like:
- Guilt
- Fear
- Anger
- Sadness
- Grief
…may turn into chronic muscle tightness, spasms, or pain syndromes.
This doesn’t mean the it isn’t physical. It is. But it also means emotional healing may be necessary for true, long-term relief.
“Pain is the body’s language when words fail.”
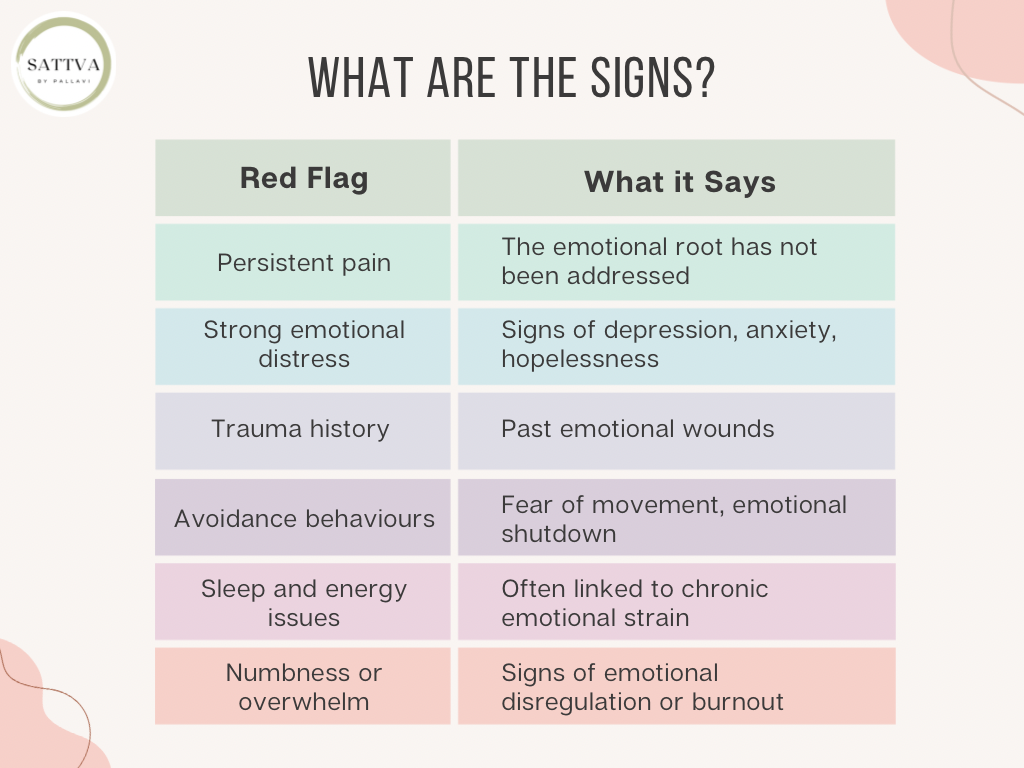
When to Refer a Client to a Psychologist
As a Mental healthcare provider, knowing when to bring in psychological expertise is key. Here are signs that it’s time to make a referral:
Activity: Pain Mapping for Clients
Encourage your clients to reflect with a gentle visual exercise:
- Draw an outline of your body.
- Mark areas where you commonly feel tension or pain.
- Beside each mark, write:
- “If this pain could talk, what might it say?”
This activity bridges physical awareness with emotional exploration—offering insight for both client and therapist.
Here is a free downloadable resource:

Conclusion: Treating the Whole Person
Pain is your body’s way of waving a flag—it wants to be heard. While physical symptoms demand attention, ignoring the emotional layer may prolong suffering.
For better outcomes, it’s important to treat both aspects. A psychologist can help decode the emotional layer, offer therapeutic tools, and build resilience—creating a more effective healing journey.
Credits: Therapist Namrata